The word hormone is derived from ancient Greek, meaning “setting in motion.” This perfectly describes the action of hormones in bringing our DNA to life. Hormones direct gene expression so that the most appropriate proteins are produced in the right amount and at the right time to optimize health and drive the positive adaptations we see during exercise training. Hormones, therefore, set in motion the process of improved athletic performance.
Out of all the hormone networks, that of the female hormones is the most complex. Each athlete will have slight differences in terms of hormone levels, timing, and biological response. This is why a personalized approach to hormone management is important.
Role of Female Hormones
As with all hormones, female hormones are vital for health and performance. The main ovarian hormones are oestrogen and progesterone. These sex steroid hormones play a crucial role in many aspects of physical and mental health. For example, female hormones support bone and soft tissue health, together with cardiovascular, neurological, and gut health. These hormones, therefore, are not just about reproduction.
Lack of Periods (Amenorrhoea)
A lack of periods is almost invariably associated with low levels of ovarian hormones. For female athletes, this often manifests as Functional Hypothalamic Amenorrhoea (FHA), which is a cessation of periods caused by an imbalance in athlete behaviors around training load and nutrition and recovery.
FHA occurs from relative energy deficiency in sport (RED-S). This is where there is a mismatch between energy intake and energy expenditure, leading to low energy availability. This causes the downregulation of many hormone networks, including those of the reproductive axis, to save energy. FHA, accompanied by low levels of female hormones, puts an athlete at risk of bone stress and soft tissue injuries, gastrointestinal issues, low mood, and, ultimately, stagnation and deterioration in performance.
Fortunately, menstrual cycles and hormone levels can be restored by addressing the balance of athlete behaviors. However, if bone health has been adversely affected by FHA, then hormone replacement therapy (HRT) can be used as a temporary measure to protect bone health. It is important to note that taking a combined oral contraceptive pill (COCP, or simply birth control pill) is not recommended to treat FHA, as the COCP masks what is going on with internal hormones and is not bone protective. To understand the difference between HRT and COCP, let’s dive into HRT.
What is Hormone Replacement Therapy (HRT)?
As the name suggests, HRT provides oestrogen and progesterone in doses to replace and bring levels of these hormones up to standard physiological levels. In contrast, COCP contains high levels of synthetic oestrogen and progesterone to suppress the production of internal female hormones. This is why COCP is a very effective form of contraception.
However, COCP will not be helpful for a woman whose female hormones — particularly oestrogen and progesterone — are already low. Bones only respond to biological oestrogen molecules and are not fooled by synthetic fakes, so the COCP is not bone-protective in FHA or in menopause.
HRT and Menopause
Menopause is a point in time when the ovaries stop producing hormones and releasing eggs. This will happen to every woman during her life — typically around 51 years of age — leaving about a third of her life to live with low levels of ovarian hormones (oestradiol and progesterone). This has an impact on quality of life and long-term health, particularly an increased risk of cardiovascular disease and osteoporosis.
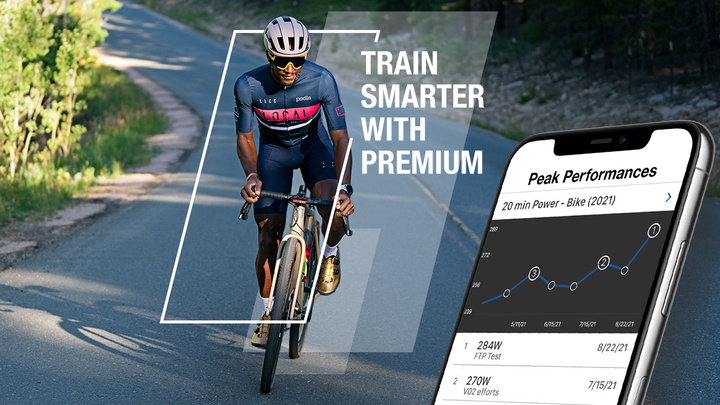
For female athletes, menopause can also mean reduced adaptation to training. Fortunately, there are ways of mitigating the effects of this decline in hormones by modifying exercise and nutrition. Specifically, increasing strength training helps maintain body composition and metabolic health; ensuring adequate protein intake will support muscle mass and function; and longer recovery from training will be necessary. Furthermore, HRT can also help maintain performance for female athletes, and it has been shown to have beneficial effects on metabolism and body composition.
Is HRT Right for Me?
It is every woman’s personal choice whether or not she wishes to take HRT. To make an informed decision, it is important to have all the facts at hand.
For instance, there is a slight increase in the risk of breast cancer after taking HRT (specifically, an extra four cases per 1,000 women aged 50 to 59 years old); but this risk isn’t any higher than that associated with taking COCP. To put this number into perspective, women who are overweight, smoke, or drink large amounts of alcohol have an increased risk of developing breast cancer by 24 extra cases. Conversely, women who exercise at least two and a half hours per week have a reduced risk of the number of breast cancer cases by seven. In fact, cardiovascular disease, not breast cancer, is the main cause of death for menopausal women — and taking HRT reduces this risk.
If you have decided to try HRT, what is the best time to start, and what are the best types of HRT? Ideally, starting HRT as soon as possible around menopause is recommended to have the most beneficial effects. This is based on troublesome symptoms such as irregular periods, mood changes, hot flashes, and brain fog.
HRT Medicines
Unless you have had a hysterectomy, you should take a combination of oestradiol and progesterone. This type of HRT is “body identical”, meaning the hormones are exactly the same as your own body produces. The best way to take oestradiol is transdermal (through the skin), either by patch or gel. I find that for athletes, the gel form is particularly convenient and practical. Individual sachets are easy to transport, and the ability to adjust dosage to symptoms is easier than with a patch.
In terms of the progesterone component, the top-shelf choice is micronized progesterone, which comes in a soft capsule called Utrogestan. This should be taken in the evening (as it can make you feel a bit drowsy) either once daily or two capsules taken in 12-day blocks every cycle/calendar month. Of course, always check the details of your medication with your prescriber.
How long should you/can you take HRT? The British Menopause Society says that there should be no arbitrary limit on how long HRT can be taken, as it all depends on the individual. In other words, a personalized approach is needed.
To quote the Vice President of the Royal College of Obstetrics and gynecology, Professor Janice Rymer, “We need to treat women as individuals, not statistics.”